The Impact of Pregnancy on Female Mental Health and Risk-Taking Behaviors
Abstract
As a risky and stressful event, pregnancy is thought to affect women’s mental health and make them risk aversive. Mental health per se also impacts risk-related decisions, further influencing pregnant women’s risk-taking propensities. This study recruited 54 pregnant women and 50 nonpregnant women and used the Perceived Stress Scale (PSS), 6-item State-Trait Anxiety Inventory (STAI-6), Patient Health Questionnaire (PHQ-9), Balloon Analogue Risk Task (BART), and delay discounting (DD) task to examine participants’ mental health and risk-taking behaviors. The results showed no significant differences in psychological states and risky decision-making between pregnant and nonpregnant women, indicating that pregnancy barely affected women’s mental health and risk-taking propensities. In addition, no correlations were found between mental health and risky behaviors. However, a negative relationship was identified between family income and DD, suggesting that people with lower family income were more likely to take risks. The experiment filled an evidence gap by pointing out that the effects of pregnancy on mental health and risk-taking were smaller than previously suggested, and mental health did not directly predict risk-taking performance. These findings could help pregnant women better evaluate their risky decisions while also allowing women in general, men, employers, and policy makers to understand the potential changes induced by pregnancy to know what to expect during pregnancy and facilitate this process.
Keywords: pregnancy, mental health, risk-taking, female
1. Introduction
Pregnancy ranks 12th, with a score of 40 out of 100, among 43 common life stressors, according to the Social Readjustment Rating Scale (SRRS) by Holmes & Rahe (1967). As an important life event, pregnancy induces both biological and psychological changes, especially in females, including weight gain, increased progesterone levels, body system changes, psychological distress, and anxiety (Figueiredo & Conde, 2011; Hodgkinson et al., 2014; Napso et al., 2018). More specifically, for instance, inevitable weight gain may cause psychological distress (Hodgkinson et al., 2014).
According to Doyle et al. (2015), 50% to 85% of women reported maternity blues between early pregnancy and postpartum. This phenomenon is worth noting due to its impacts on mothers-to-be and fetuses as well as its prevalence. For example, high levels of prenatal maternal stress (PNMS) may increase the susceptibility of the offspring to delays in cognitive or emotional development and abnormal neurodevelopment, which could evolve into psychological problems later in life (Allison et al., 2011; Ceulemans et al., 2021; Davenport et al., 2020; Miguel et al., 2019). Studies assessing mothers who were pregnant during a natural disaster in Canada found that PNMS was related to lower cognitive and language abilities in their offspring and may predict autism traits (Laplante, et al., 2008; Walder et al., 2014). Luckily, increasing social support, peer support, paternal participation, physical exercise, drug therapy, cognitive behavioral therapy, etc. can buffer the negative impact of mental distress on both mothers and fetuses (Bahk et al., 2015; Field, 2017; Kita et al., 2019).
Risk factors for maternal mood distress include domestic violence, a family history of mental illness, parenting stress, low perceived social support, high perceived stress, unplanned pregnancy, traumatic life events, and catastrophic events. (Biaggi et al., 2016; Chhabra et al., 2020; Field, 2017; Kita et al., 2019; Li et al., 2017; Sheeba et al., 2019). The COVID-19 pandemic is one of them. Under its influence, people were experiencing extra stress stemming from concerns about their health, medical resources, financial stability, etc. (Ceulemans et al., 2021; Subbaraman, 2021). In particular, families bearing new babies may undergo more stress because of external unpredictable factors such as fear of the virus, difficulties going to a hospital for a screening test, and lack of data regarding vaccines (Subbaraman, 2021). However, when comparing the susceptibility to psychological disorders between pregnant and nonpregnant people, researchers have come to somewhat counterintuitive conclusions. On the one hand, Liu et al. (2020) compared two cities, Wuhan and Chongqing, and found that pregnant women in Wuhan, the epicenter, were more anxious. Other studies identified a similar trend: a high prevalence rate of mental disorders, including maternal depression and anxiety, among pregnant and postpartum women during the pandemic (Ceulemans et al., 2021; Davenport et al., 2020; Yan et al., 2020). On the other hand, despite its high prevalence, Borba et al. (2012) reviewed 25 articles on common mental disorders (CMDs) among pregnant and nonpregnant women and found no differences in prevalence and incidence. Another systematic review by the Effective Health Care Program (2019) from the U.S. Department of Health & Human Services had similar findings. Moreover, Zhou et al. (2020) suggested that in comparison with nonpregnant women, pregnant women were more resilient to psychological problems related to COVID-19. In short, conflicting evidence has suggested that pregnant women may not be as vulnerable to mental disorders as previously expected.
In addition to the influences of pregnancy on psychological health, researchers have also been interested in how pregnancy affects risky decision-making, the trade-off between immediate positive outcomes with greater negative consequences and long-term benefits with some costs (Buelow, 2020). To pregnant women, decisions that need to be made can range from whether to keep the baby, quit their job, and move to a larger house to choices of prenatal care, aneuploidy screenings, and methods of delivery (Chen et al., 2020; Liu et al., 2020). Past studies suggested that both mental health and pregnancy could influence risk-related decisions, leading to the possible formation of mediating or moderating relationships among the three variables. In a mediation model, pregnancy may not directly affect risk-taking propensities, but psychological problems induced by pregnancy may change risk-taking preferences. However, in a moderation model, pregnancy directly impacts risk-taking behaviors, while mental health modifies the strength of this relationship. A review article revealed that stress affected risky decisions by altering its mechanisms, such as changing sensitivity to reward and punishment and increasing reliance on automated responses (Starcke & Brand, 2012). It has been shown that people with anxiety tended to avoid risk, and those with depression were reluctant in terms of sensation seeking (Bishop & Gagne, 2018). Sensation seeking, along with impulsivity, are two widely used indicators of risk-related behaviors (Chen et al., 2020). Pregnant women were shown to be risk aversive and scored lower in sensation seeking, but their impulsivity scores were not different from those of nonpregnant women (Chen et al., 2020). Similarly, Li et al. (2015) argued that pregnant women focused on long-term benefits and were future-oriented as a means to protect their offspring and transition to their new roles as mothers (Sevin & Ladwein, 2008). They termed this phenomenon “maternal mind”. Interestingly, not only pregnant women showed these changes; by viewing relevant materials, nonpregnant women could enter similar mental conditions as pregnant women and demonstrated similar changes (Li et al., 2015).
From an evolutionary perspective, pregnancy itself is risky; to ensure its success, mammals will change their behaviors (Li et al., 2016). Specifically, these behaviors are identified as self-regulation or self-control in humans. For example, pregnant women may quit smoking, start saving money, and exercise regularly to secure positive pregnancy outcomes (Li et al., 2016; Moran et al., 2006; Savin & Ladwein, 2008). Bell et al. (2013) studied teenage pregnancies and argued that those who decided to terminate the pregnancy had a clearly developed plan for the future, whereas those who continued with the pregnancy paid more attention to daily living. The authors proposed that this may be due to different levels of internal control—teenagers who decided to end an unwanted pregnancy displayed higher senses of internal control. Nonetheless, in general, unplanned pregnancy as a risk factor still poses a negative impact on maternal mental health (Bahk et al., 2015).
In summary, previous research has examined the mental health and risk-taking behaviors of pregnant women compared to those of nonpregnant women but came to divergent conclusions. Although some studies claimed an effect of pregnancy on mental health or risk-taking, at least to the author’s knowledge, a mediation or a moderation relationship among these three variables has not been evaluated. Therefore, the purpose of the current study was to compare mental health between pregnant and nonpregnant women and to understand the impact of pregnancy and mental health on risky decision-making. The author hypothesized that pregnant women would have higher levels of mental distress than nonpregnant women, that pregnancy induces risk aversion, and that there is a significant effect of mental health on risk-taking decisions.
2. Method
2.1 Participants
The present study recruited 54 pregnant women aged 20 to 35 years old (Mage=27.89, SD=3.47) in the obstetrics department of a public hospital in Foshan, a second-tier city located in Southern China, and 50 nonpregnant women aged 18 to 56 years old (Mage=30.98, SD=10.20) between August 2nd and 20th, 2021. The researcher selected pregnant women who were attending the hospital for fetal heart rate monitoring or a pregnancy education session to ensure that they had enough time to complete the tasks. Meanwhile, a small portion of the nonpregnant participants was recruited from the same hospital, consisting of mothers accompanying their pregnant daughters. The remaining nonpregnant participants were recruited through convenience sampling. The experiment was approved by the hospital before data collection.
2.2 Instruments
2.2.1 Perceived Stress Scale (PSS)
Stress was measured using the 14-item Perceived Stress Scale (PSS). The original scale was developed by Cohen et al. (1982), and its Chinese version (CPSS), developed by Yang and Huang (2003), showed good reliability (Cronbach’s alpha=0.71) and validity among both pregnant and nonpregnant populations (Huang et al., 2020; Lau, 2012; Solivan et al., 2015).
The PSS consisted of a negative (e.g., “how often have you felt nervous and ‘stressed’”) and a positive subscale (e.g., “how often have you felt that things were going your way”). The participants were asked to rate their feelings and thoughts on these statements for the past month based on a 5-point Likert scale ranging from 1=“never” to 5=“very often”; higher scores meant more perceived stress.
2.2.2 Patient Health Questionnaire (PHQ-9)
Levels of depression were assessed using the 9-item Patient Health Questionnaire (PHQ-9) by Kroenke et al. (2001). O’Connor et al. (2016) reviewed 78 articles evaluating depression screening instruments among pregnant and postpartum women and suggested that the PHQ was a reliable tool. Specifically, two items (“little interest or pleasure in doing things” and “feeling down, depressed or hopeless”) from the PHQ demonstrated good sensitivity in screening depression in pregnancy (Bennett et al., 2008; Breedlove & Fryzelka, 2011; Sidebottom et al., 2012).
Overall, the PHQ consisted of 9 symptoms, and the participants rated the frequency of occurrence of these symptoms over the past two weeks on a 4-point Likert scale ranging from 0=“not at all” to 3=“nearly every day”. Higher scores indicated greater depression severity. The present study employed the Chinese version of the PHQ, developed by Wang et al. (2014), which exhibited good reliability (Cronbach’s alpha=0.86) and validity among the Chinese population (Liu et al., 2007). Furthermore, the PHQ has been employed among pregnant women in China and has shown good reliability (Cronbach’s alpha=0.87) (Zhou, Wang, et al., 2021).
2.2.3 Six-item Spielberger State-Trait Anxiety Inventory (STAI-6)
The six-item shortened version of the State-Trait Anxiety Inventory (STAI-6) was used to evaluate levels of anxiety. The original STAI was developed by Spielberger et al. (1983) and consisted of 40 items. Brunton et al. (2015) reviewed 60 studies on scales measuring pregnancy anxiety and revealed that the STAI was one of the most widely used instruments.
The STAI-6 was created by Marteau and Bekker (1992), comprise 6 items from the state form (STAI-S), and has good reliability (Cronbach’s alpha=0.82) and validity. The STAI-6 was tested with 223 pregnant women by Marteau and Bekker, illustrating possible application in this population. Bayrampour et al. (2014) demonstrated that the STAI-6 is also reliable with perinatal women. Moreover, Sinesi et al. (2019) specifically noted in their review of 22 studies about anxiety scales used in pregnancy and suggested that the STAI-6 had a high correlation with the STAI-S.
In the current experiment, the Chinese version of the STAI developed by Zheng et al. (1993) was employed. The STAI-6 has three positive (e.g., “I feel calm”) and three negative statements (e.g., “I am tense”), and the participants selected how much these statements described their present feelings on a 4-point Likert scale ranging from 1=“not at all” to 4=“very much”. People with higher levels of anxiety score higher.
2.3 Behavioral Tasks
2.3.1 Balloon Analogue Risk Task (BART)
The Balloon Analog Risk Task (BART) was used to measure participants’ risk-taking behaviors (Lejuez et al., 2002). An advantage of the BART was that it required balancing between gain and loss, which resembles real-world risk-taking and is known as sequential risk-taking (Wallsten et al., 2005). As potential earnings increased, the risk of losing also increased. The participants were asked to press a button to pump air into the balloon, and they would receive monetary rewards for each pump. However, the balloon could burst at any time, and all rewards gained in that particular trial would be taken away once it burst. The participants were instructed to collect as much money as possible while avoiding bursts. Based on previous research, participants gradually learn and optimize their performance by finding a comfort point to stop pumping and stick to it (Lejuez et al., 2002; Zhou, Myung, et al., 2021).
The present study included 30 trials of the BART. In each trial, the balloon burst after 1 to 20 pumps, with an average break point of 10 pumps and SD of 5.05. The chances of bursting were randomized across trials. The participants needed to pump at least once; then, they could either continue to pump or collect the rewards. Each pump resulted in a ¥10 virtual monetary award. On the screen, as shown in Figure 1, the “Collect” button and “Pump” button were arrayed next to each other at the bottom. Rewards for the current trial and the cumulative reward are shown on the left. In the top-right corner, the participants could see the trial number. When the balloon burst, a “bang” sound played. Risk-taking behavior was measured by the average number of pumps on unexploded trials, which is called adjusted pumps (Lejuez et al., 2002).
Figure1
Screenshot of the Balloon Analogue Risk Task
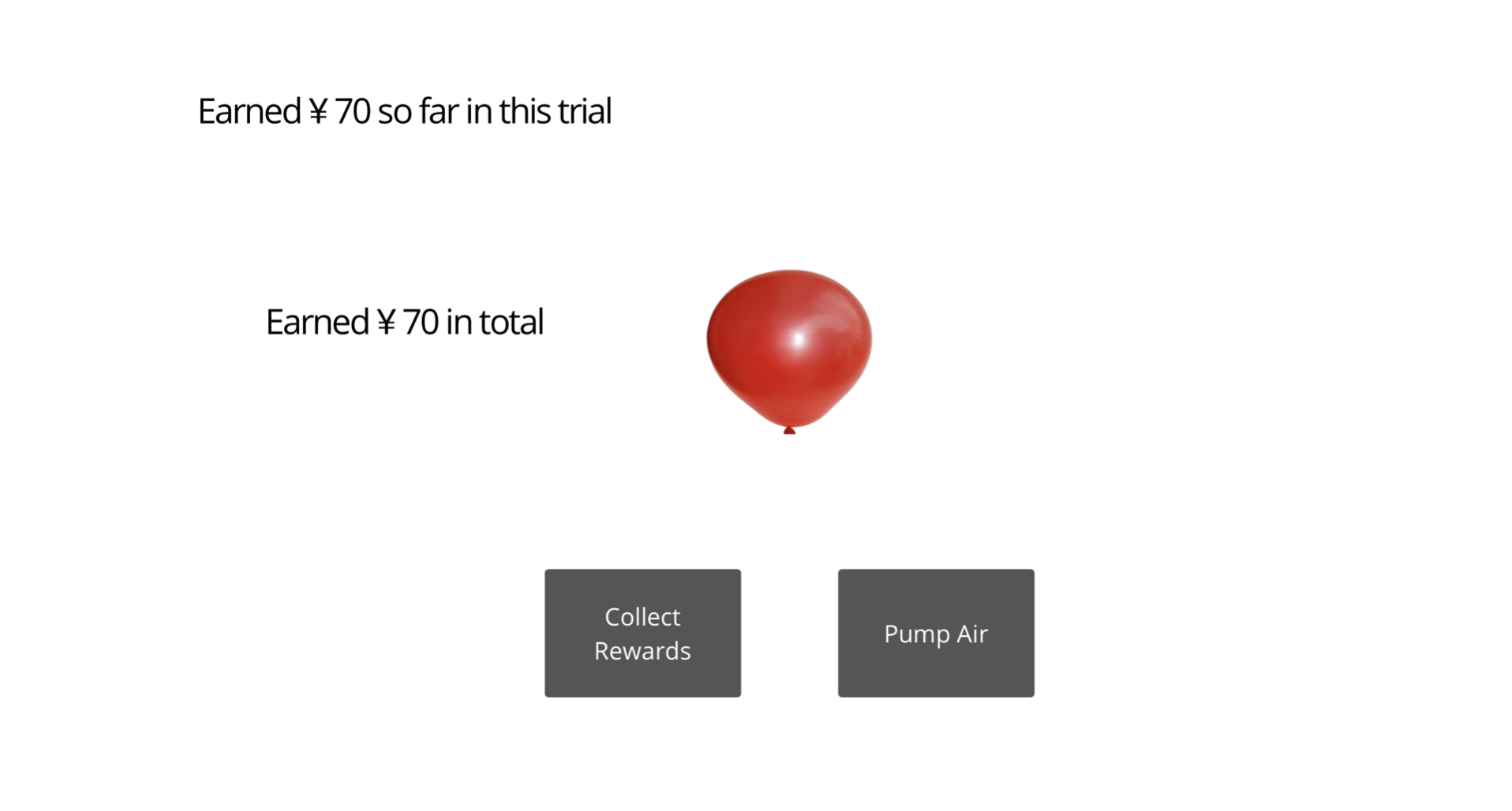
Note. In the actual experiment, the screen displayed only Chinese.
2.3.2. Delay Discounting Task (DD)
While the BART emphasized sequential risk-taking behaviors, the DD paradigm emphasized another aspect of risky decision-making: delay of gratification. Although similar to the famous “marshmallow experiment” conducted by Mischel et al. (1972) to study children’s delayed gratification behaviors, the DD paradigm in this study focused on monetary rewards. The participants could receive a reward now or wait for a larger reward later, as shown in Figure 2. To measure these decisions, the discounting rate parameter (k) was introduced. There are multiple ways to calculate the discounting rate, and the researcher used the discounting rate provided by the hyperbolic function: V=A/(1+kD) (Mazur, 1987). In this formula, V was the immediate reward, A was the delayed reward, and D was the delay in days.
The current study used the 21-item Monetary Choice Questionnaire (MCQ) created by Kirby and Maraković (1996). Since the participants in this experiment were Chinese but the original questionnaire used USD, the author converted the monetary values into RMB while keeping k the same. The order of trials was randomized across participants. The results were calculated with an Excel automated scorer by Kaplan et al. (2016); greater values of kreflected greater impulsivity in risk-taking, suggesting that people preferred immediate rewards.
Figure 2
Screenshot of the Delay Discounting Task
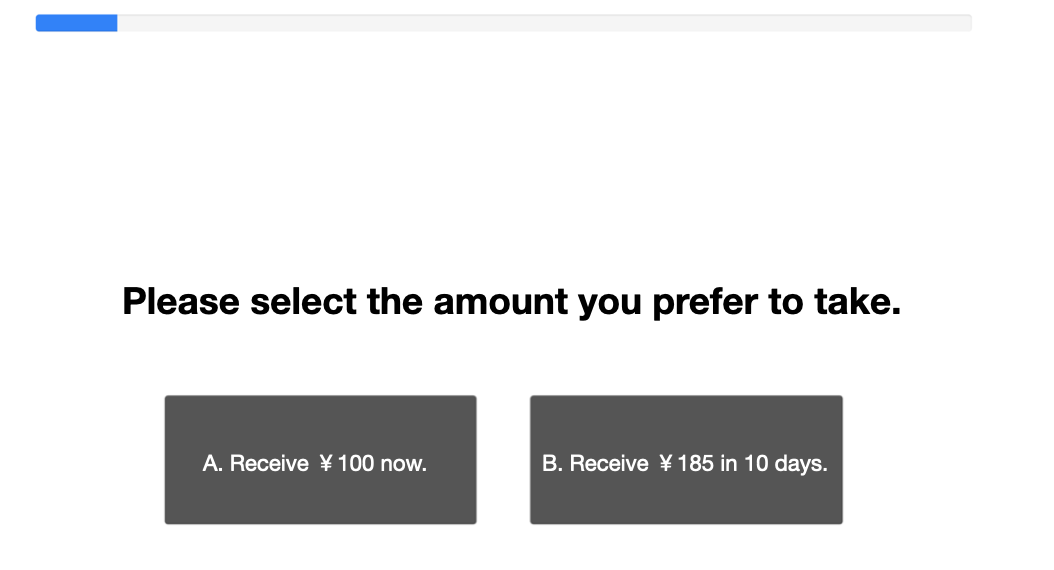
Note. In the actual experiment, the screen displayed only Chinese.
2.4 Procedures
The experiment was created in Gorilla Experiment Builder (www.gorilla.sc) and consisted of eight demographic questions, the STAI-6, PSS, and PHQ questionnaires, and the BART and DD task (Anwyl-Irvine et al., 2018). The BART was adopted from Gorilla open material shared by Pike et al. (2021). A QR code was generated using the link, and all participants accessed the experiment through scanning the link.
2.5 Data analysis
Data were analyzed using Microsoft Excel (2019) for Mac and RStudio (RStudio Team, 2020). The levels of perceived stress, anxiety and depression, sequential risk-taking behaviors, and delayed gratification behaviors were compared between the pregnant and nonpregnant groups using descriptive statistics and t-tests. The relationships between mental health (i.e., perceived stress, anxiety, and depression) and risk-taking behaviors were measured using correlation tests and linear regression. Regression analyses were also employed to determine whether sociodemographic differences such as age, marital status, number of pregnancies, family income, and education could predict the mental health and risk-taking decision outcomes.
3. Results
3.1 Demographics
Table 1 presents the demographic characteristics of the 104 participants. Overall, the nonpregnant group (n=50) was older than the pregnant group (n=54), who were mainly in the 2nd or 3rd trimester. The levels of education of the nonpregnant group were higher than those of the pregnant group (p<0.01). The pregnant group was primarily married. Unmarried participants in the nonpregnant group all reported having a partner
Table 1
Demographic Characteristics of the Participants (n=104)
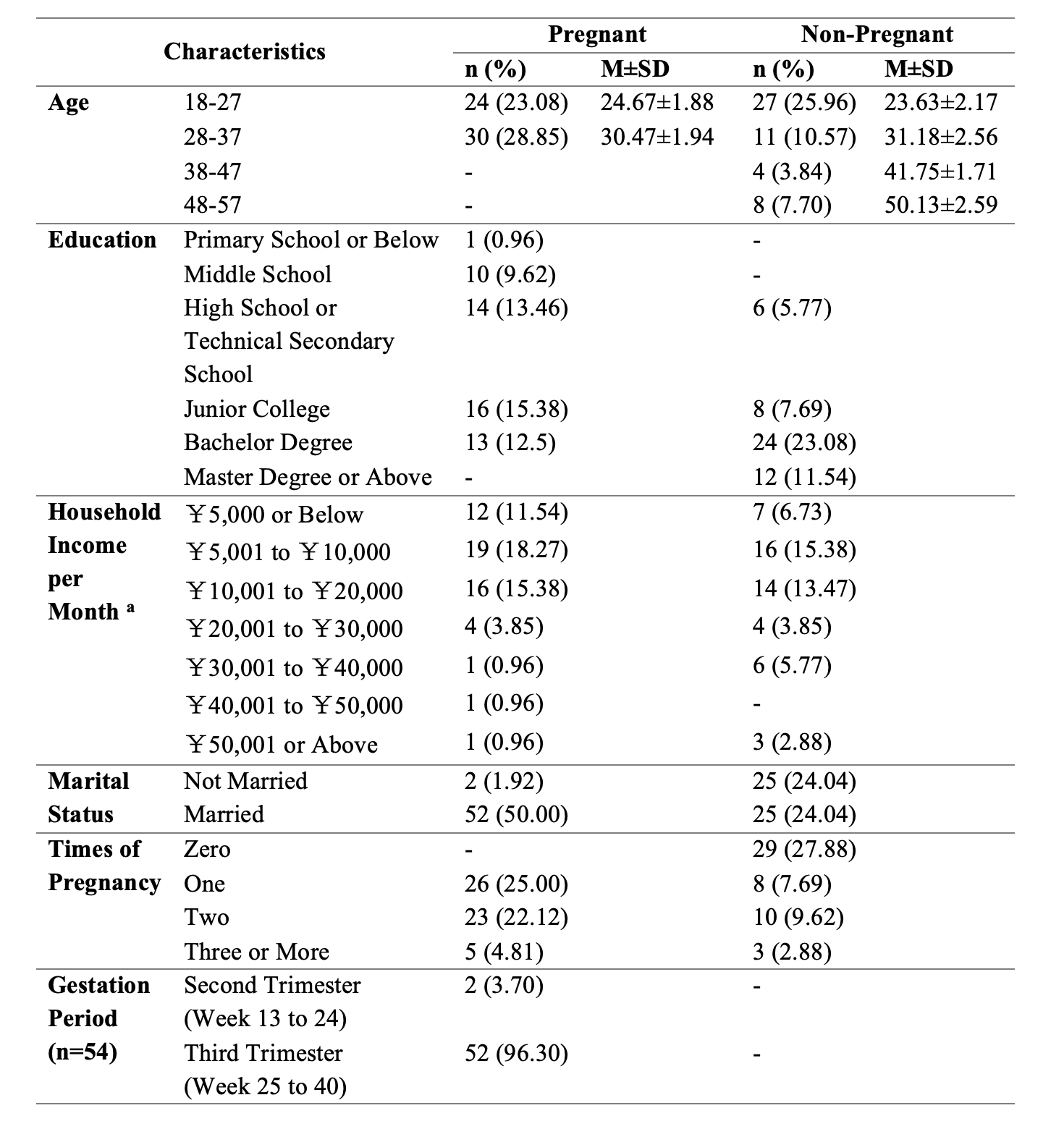
Note. All participants are females.
a 100 RMB equal 15 USD approximately.
3.2 Mental Health
The descriptive mental health outcomes for the pregnant and nonpregnant groups are shown in Table 2. The PSS scores ranged from 14 to 70, with cutoff scores of 43 and 47, respectively. The STAI-6 scores ranged from 6 to 24 with a cutoff at 16.5, and the PHQ scores ranged from 0 to 27 with cutoffs at 5, 10, 15, and 20. The differences between pregnant women and nonpregnant women in the levels of perceived stress, anxiety, and depression are shown in Figure 3. There were no significant differences between the mental states of the two groups (p>0.05).
Table 2
Mental Health States of the Pregnant and the Non-Pregnant Groups
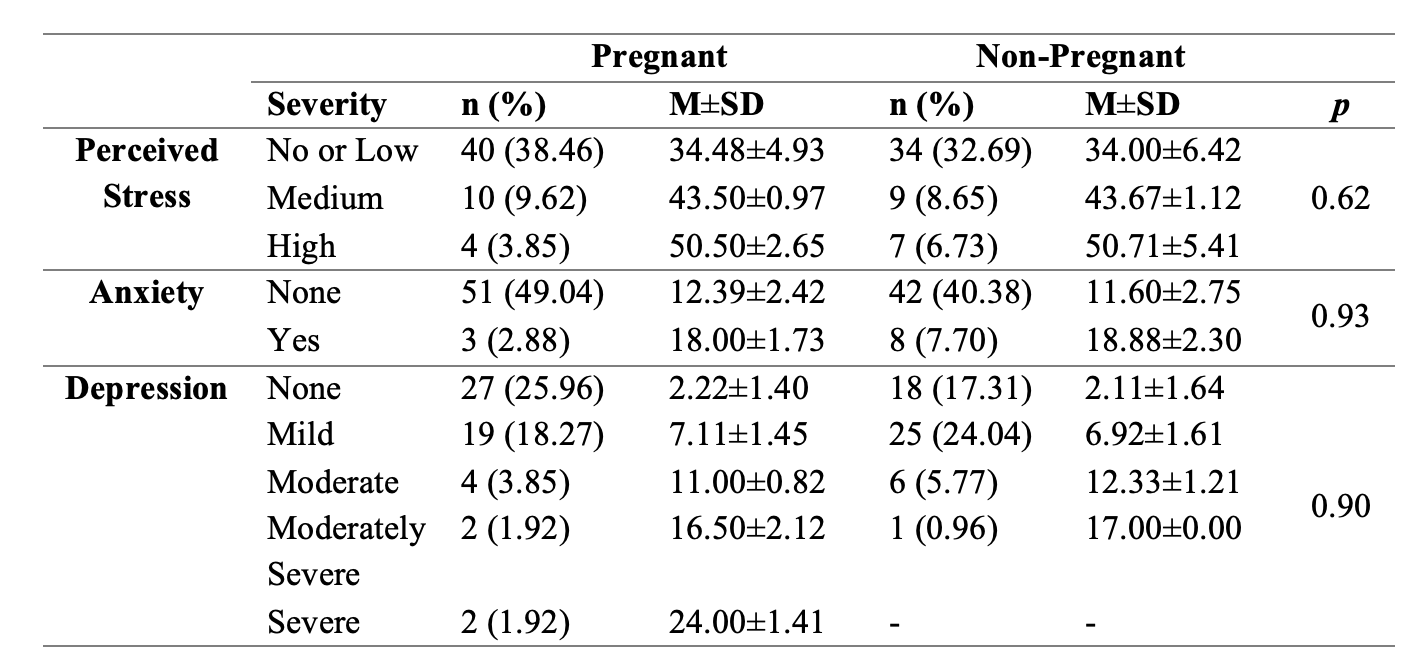
Figure 3
Levels of Perceived Stress, Anxiety, Depression, Mean Scores of Adjusted Pumps, and Overall k of the Pregnant compared to the Non-Pregnant Groups
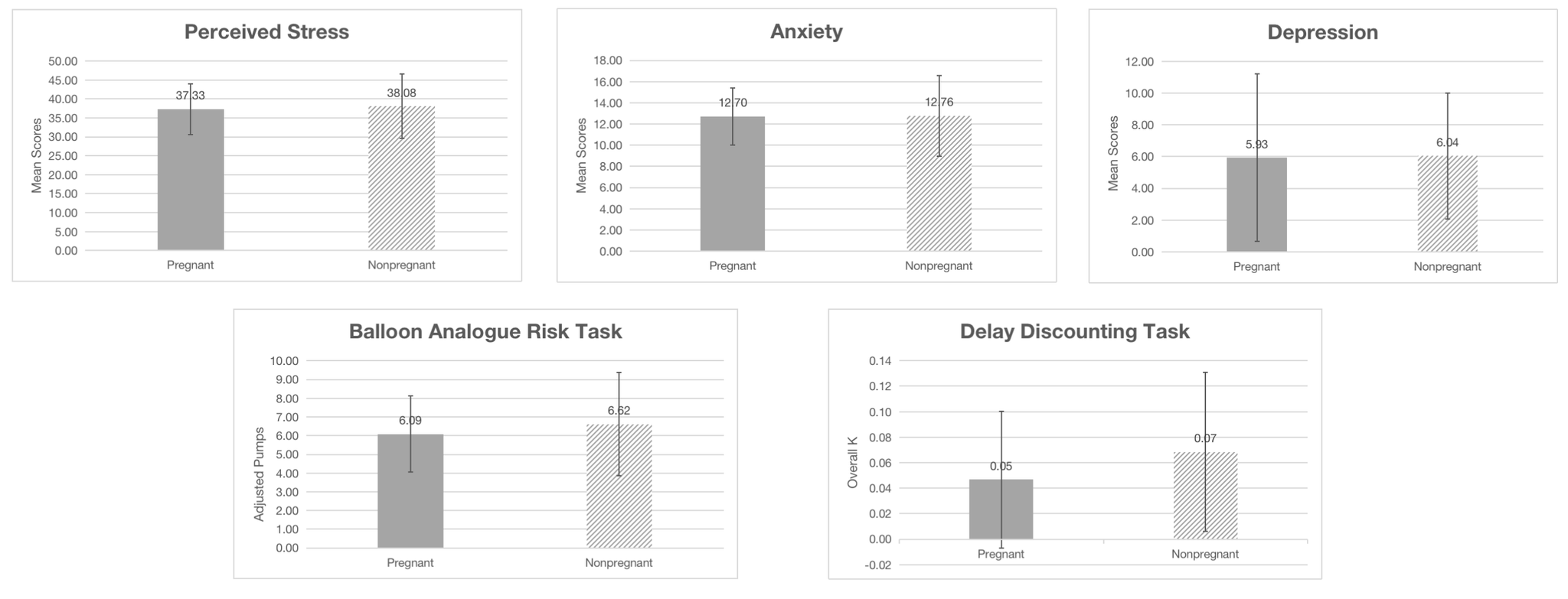
Note. Error bars correspond with the standard error of the mean.
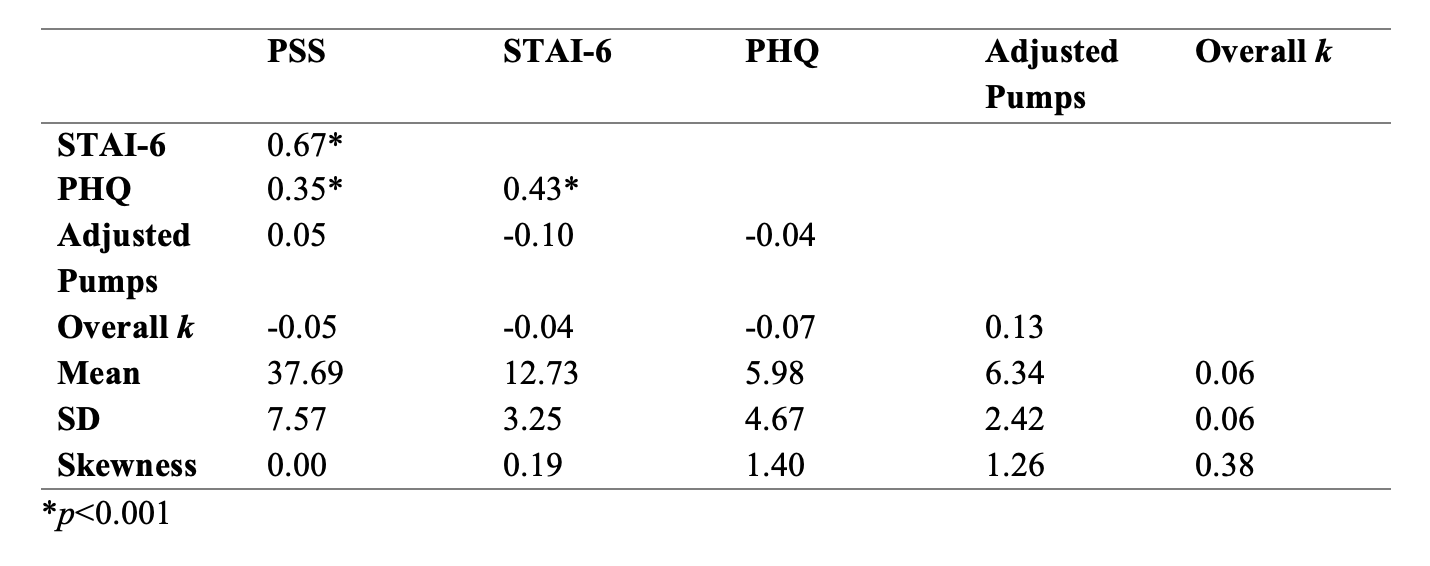
The descriptive statistical results and the correlations among the three scales and two tasks are shown in Table 3. The PSS and STAI-6 show a moderately strong positive correlation (r (102) =0.67, p<0.001), while the PHQ had moderately weak positive correlations with the PSS (r (102) = 0.35, p<0.001) and STAI-6 (r (102) =0.43, p<0.001). There were no significant correlations between mental health and BART or DD task performance.
Table 3
Correlations of Main Variables
3.3 Risk-Taking Behaviors
The differences in the BART and DD outcomes between the two groups are illustrated in Figure 3 (p>0.05). Regression analysis suggested a relationship between family income and DD. The researcher turned the 7 levels of family incomes into numeric factors 1 to 7, and the result, shown in Figure 4, shows that family incomes accounted for 4% of the variance in the DD task performance (F (1, 102) =4.68, p<0.05)
Figure 4
Scatterplot with the Regression Line of Family Income and Delay Discounting Task Outcomes
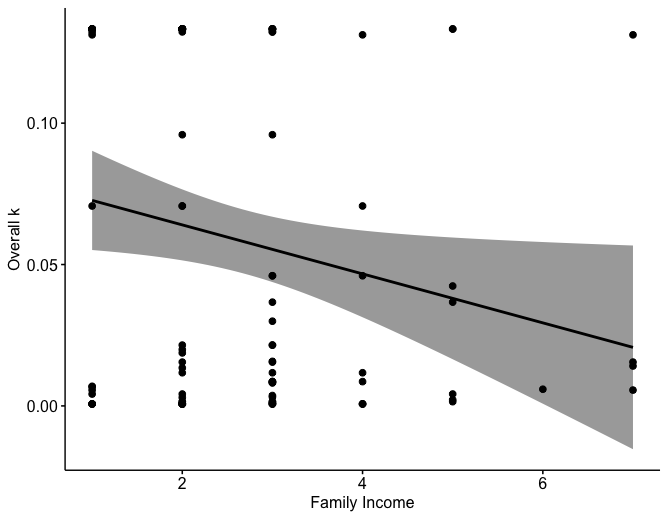
Note. Shaded area corresponds with confidence interval (R2=0.04, p<0.05).
4. Discussion
There were no significant differences between the psychological states of pregnant and nonpregnant women. Their risk-taking propensities were also not different from each other. An impact of mental health problems on risk-taking decisions was not found. Thus, neither a mediation nor a moderation relationship was supported.
The reason why a higher prevalence of mental distress among pregnant women was not supported may be due to differing recruitment policies. The pregnant women were recruited from a local city’s hospital, while the nonpregnant women were recruited through convenience sampling. There were significant differences in education levels between these two groups (p<0.01). Both the median and the mode of the pregnancy group were at the junior college level, while for the other group, they were at the bachelor’s degree level. Although education per se does not change people’s mental health, previous studies have argued that a sense of control, resilience, and likelihood of taking actions all mediate the relationship between education and psychological states (Niemeyer et al., 2019; Steele et al., 2007). When comparing the scores of perceived stress with a Chinese community sample (n=9507, MPSS=27.5, SD=7.1), the score for the sample in the present study (23.70±7.57) was lower than that for the community sample (Huang et al., 2020). Since this experiment used a Likert scale from 1 to 5, the mean score was subtracted by 14 to match the community sample. Wang et al. (2014) used a Chinese population (n=1045) and calculated PHQ scores with a mean of 3.3 and standard deviation of 4.0, which was lower than that in this experiment (5.98±4.67). Yirmiya et al. (2021) studied 1114 pregnant women and 256 nonpregnant women and found PHQ-2 scores of 1.3±1.41 and 1.52±1.56, respectively. The PHQ-2 includes the first two items of the PHQ-9, and the PHQ-2 result for this study was 1.43±1.35. Sidebottom et al. (2012) found that 18.4% of their sample of pregnant women (n=745) scored higher than 10 on the PHQ-9, while this study found 14.4%. Regarding the STAI-6, Marteau and Bekker (1992) assessed 200 pregnant women with prorated scores of 37.5±8.7, compared to 38.10±8.10 in the current study. Hence, this study’s sample had less perceived stress and similar levels of depression and anxiety compared to other samples. Consequently, there are two possibilities: a relatively small sample size did not capture the true mental health situations of the population, or there were no consistent conclusions, and pregnancy accounts for only a small amount of variance in women’s mental health outcomes.
This experiment also did not support an effect of pregnancy on risky decision-making. On the one hand, BART performance has been positively correlated with risk-related behaviors, such as addiction, gambling, alcoholism, and substance abuse (e.g., Ashenhurst et al., 2014; Banducci et al., 2015 Lejuez et al., 2002). However, it has barely been used among pregnant populations. In fact, risk-related behavioral tasks have rarely been applied to this population in general. Nevertheless, Chen et al. (2020) used the Columbia card task (CCT) and found that pregnant women were more reluctant to take risks. However, the impact of pregnancy on risk-taking from an evolutionary perspective has barely been mentioned in previous research. Furthermore, sex differences in risk-taking propensities have been reported; Lighthall et al. (2008) argued that under stress, men increased risk seeking, while women decreased risk seeking. Harris et al. (2006) also supported this sex difference in risk-taking. Since this experiment focused on females, the variances within the group may be small.
On the other hand, the DD task examined the impact of pregnancy on long-term considerations. Previous research has pointed out that mothers-to-be were more likely to regulate their behaviors and save resources to secure the survival of their offspring (Li et al., 2016; Moran et al., 2006; Savin & Ladwein, 2008). Li et al. (2015) found a significant effect of pregnancy on DD. Nonetheless, although not found in this experiment, Niemeyer et al. (2019) showed that DD followed gradients along education levels. In this experiment, the pregnant group had a significantly lower education level (p<0.01). Therefore, the potential influences of pregnancy on DD may have been mitigated by education. Moreover, this study’s results suggested a negative relationship between family income and DD, although no differences were found in family income between the two groups. de Matta et al. (2012) found that people with lower incomes showed greater rates of DD, i.e., were more impulsive. Other studies have also identified lower education and income, along with a lower age, to be associated with greater discounting rates (Oshri et al., 2019; Reimers et al., 2009).
Mental health did not impact risk-taking behaviors in this study. In addition to the small sample size, Starcke and Brand (2012) argued that stress, one aspect of mental health examined in the experiment, was not behaviorally connected to risky decision-making but was connected at a neural level through reducing reward and punishment learning. Additionally, Pailing and Reniers (2018) reported contradictory correlations between depressive symptoms and risk-taking: some were positive, while others were negative. Regarding anxiety, Kusev et al. (2017) suggested that anxiety was related to risk aversion; meanwhile, Hartley and Phelps (2012) identified anxiety as “a state of sustained fear” and argued that trait anxiety, worry, and social anxiety could all predict risk aversive behaviors in the BART. However, Pailing and Reniers (2018) mentioned that people with social anxiety may take risks to increase acceptance. Thus, although some studies support a predictive relationship between mental health and risk-taking, its effects may differ when different subcategories of mental health are examined. Additionally, protective factors, such as resilience, optimism, and psychological interventions, could mitigate the influences of psychological disorders on behavioral outcomes.
As mentioned above, this experiment was limited by different recruitment policies. The testing environments also differed: the pregnant group completed the tasks in a hospital, while the nonpregnant group completed the tasks in places of their choosing. This may have led to some biases in the results. For instance, the pregnant group may have been more anxious or impatient. Additionally, the sample size was small, and there were differences in socioeconomic status between the two groups, which introduced extra variables into the study.
Therefore, future studies should recruit a larger, more diverse sample and avoid places that could bias the results, such as hospitals. The mental health of pregnant women in the 1st and 2nd trimesters and new mothers after childbirth are also worth investigating. Moreover, prospective studies can use other behavioral tasks, such as the CCT for comparison to the BART. Positive traits or protective factors help pregnant women buffer the negative influences induced by pregnancy or mental problems and are worth exploring. Furthermore, the relationships among pregnancy, mental health, and risk-taking are still worth investigating. Overcoming the limitations of sample size and recruitment methods, future studies could collect more comprehensive data or utilize a meta-analysis method to evaluate the relationships. In this experiment, the question regarding whether the pregnancy was planned was not addressed; since unplanned pregnancy itself is risky, prospective research could compare the risk-taking propensities of participants with unplanned pregnancies to those with planned pregnancies.
Another important aspect is how pregnancy affects men. Women are not sole warriors facing pregnancy. An article reported that 7 to 10% of fathers-to-be were affected by perinatal mood disorders, and their emotions also affected the children (Madsen, 2019). Moreover, a meta-analysis suggested that maternal depression, marital distress, and parental stress were significant risk factors for paternal perinatal depression and anxiety (Chhabra et al., 2020). It seems that there is not much that fathers-to-be can do during pregnancy, but their emotions have been shown to influence their pregnant partners, emphasizing the importance of psychological health for both women and their partners (Ahorsu et al., 2020; Kazemi et al., 2021; Figueiredo & Conde, 2020). Consequently, future research could examine the impact of pregnancy on males’ mental health, as well as how it affects couples as a whole. Whether there are sex differences in risk-taking and whether pregnancy makes males more risk aversive are interesting topics as well.
Overall, this study filled an evidence gap by showing that the impacts of pregnancy on mental health and risk-taking decisions were smaller than what previous research indicated. It also addressed the complicated mechanisms of how mental health affects risk-taking and how sociodemographic status could change risk-related results. Unlike men, many women who choose to have babies may experience pregnancy discrimination, as work-family balance has long been identified as a major conflict in women’s careers. Russell and Banks (2011) suggested that pregnant women experienced various forms and severities of discrimination in the workplace, including receiving unsuitable work or workloads, being subject to unpleasant judgments, being poorly treated, being discouraged from receiving antenatal instructions, and so on. A more recent study also supported the prevalence of this phenomenon, although the situation has improved (Becker et al., 2019). One implication of the results was that pregnancy did not affect women much at the psychological level; women may be tougher or more resilient to mental distress than expected based on the literature. Furthermore, the results regarding risk-taking could help pregnant women better evaluate their risk-related choices. Decisions on prenatal care, food, antenatal instructions, career, and living conditions may all be necessary during pregnancy. This study provided evidence that pregnant women were capable of making sound decisions. Hence, pregnant women should be more confident in their informed decisions. Meanwhile, studies focusing on more realistic scenarios, such as medical decisions, high-risk pregnancy, and fetal safety, have pointed out that real-world risky decision-making was filled with competing interests between mothers and babies, health professionals and their own experience, uncertainty and excitement, which highlights the need to improve informed decision-making processes for pregnant women (Farrell et al., 2011; Lee et al., 2015; Lyerly et al., 2007; McDonald et al., 2011). Thus, finally, the conclusions are useful for fathers-to-be, employers, and policy makers, allowing them to better understand how pregnancy psychologically and behaviorally affects women and to facilitate this process.
References
Ahorsu, D.K., Imani, V., Lin, CY., Timpka, T., Broström, A., Updegraff, J.A., Årestedt, K., Griffiths, M.D., & Pakpour, A.H. (2020). Associations Between Fear of COVID-19, Mental Health, and Preventive Behaviours Across Pregnant Women and Husbands: An Actor-Partner Interdependence Modelling. International Journal of Mental Health and Addiction. https://doi.org/10.1007/s11469-020-00340-x
Allison, S.J., Stafford, J. & Anumba, D.O. (2011). The effect of stress and anxiety associated with maternal prenatal diagnosis on feto-maternal attachment. BMC Women's Health, 11, 33. https://doi.org/10.1186/1472-6874-11-33
Anwyl-Irvine, A.L., Massonié J., Flitton, A., Kirkham, N.Z., Evershed, J.K. (2019). Gorilla in our midst: an online behavioural experiment builder. Behavior Research Methods. Doi: https://doi.org/10.3758/s13428-019-01237-x
Ashenhurst, J. R., Bujarski, S., Jentsch, J. D., & Ray, L. A. (2014). Modeling behavioral reactivity to losses and rewards on the Balloon Analogue Risk Task (BART): Moderation by alcohol problem severity. Experimental and Clinical Psychopharmacology, 22(4), 298–306. https://doi.org/10.1037/a0036837
Bahk, J., Yun, S.C., Kim, Y., & Khang, Y.H. (2015). Impact of unintended pregnancy on maternal mental health: a causal analysis using follow up data of the Panel Study on Korean Children (PSKC). BMC Pregnancy Childbirth, 15(85). https://doi.org/10.1186/s12884-015-0505-4
Banducci, A.N., Felton, J.W., Dahne, J., Ninnemann, A., & Lejuez, C.W. (2015). Maternal risk taking on the balloon analogue risk task as a prospective predictor of youth alcohol use escalation. Addictive Behaviors, 49, 40-45. https://doi.org/10.1016/j.addbeh.2015.05.011
Bayrampour, H., McDonald, S., Fung, T., Tough, S. (2014). Reliability and validity of three shortened versions of the State Anxiety Inventory scale during the perinatal period. Journal of Psychosomatic Obstetric & Gynecology, 35(3), 101-107. doi: 10.3109/0167482X.2014.950218.
Becker, S.O., Fernandes, A., & Weichselbaumer, D. (2019). Discrimination in hiring based on potential and realized fertility: Evidence from a large-scale field experiment. Labour Economics, 59, 139-152. https://doi.org/10.1016/j.labeco.2019.04.009
Bell, E. R., Glover, L., & Alexander, T. (2014). An exploration of pregnant teenagers' views of the future and their decisions to continue or terminate their pregnancy: implications for nursing care. Journal of clinical nursing, 23(17-18), 2503–2513. https://doi.org/10.1111/jocn.12431
Bennett, I. M., Coco, A., Coyne, J. C., Mitchell, A. J., Nicholson, J., Johnson, E., Horst, M., & Ratcliffe, S. (2008). Efficiency of a two-item pre-screen to reduce the burden of depression screening in pregnancy and postpartum: an IMPLICIT network study. Journal of the American Board of Family Medicine: JABFM, 21(4), 317–325. https://doi.org/10.3122/jabfm.2008.04.080048
Biaggi, A., Conroy, S., Pawlby, S., & Pariante, C.M. (2016). Identifying the women at risk of antenatal anxiety and depression: A systematic review. Journal of affective disorders, 191, 62–77. https://doi.org/10.1016/j.jad.2015.11.014
Bishop, S. J., & Gagne, C. (2018). Anxiety, Depression, and Decision Making: A Computational Perspective. Annual review of neuroscience, 41, 371–388. https://doi.org/10.1146/annurev-neuro-080317-062007
Borba, P., Zambaldi, C.F., Cantilino, A., & Sougey, E.B. (2012). Common mental disorders in mothers vs. infant and obstetric outcomes: a review. Trend Psychiatry Psychotherapy, 34(4), 171-177. https://doi.org/10.1590/S2237-60892012000400002
Breedlove, G., & Fryzelka, D. (2011). Depression screening during pregnancy. Journal of Midwifery & Women’s Health, 56, 18-25. doi:10.1111/j.1542-2011.2010.00002.x
Brunton, R.J., Dryer, R., Saliba, A., & Kohlhoff, J. (2015). Pregnancy anxiety, a systematic review of current scales. Journal of Affective Disorders, 176, 24-34. http://dx.doi.org/10.1016/j.jad.2015.01.039
Buelow, M.T. (2020). An introduction to risky decision making. In Buelow, M.T. (Ed.). Risky Decision Making in Psychological Disorders (pp. 3-13). Academic Press. https://doi.org/10.1016/B978-0-12-815002-3.00001-2.
Ceulemans, M., Foulon, V., Ngo, E., Panchaud, A., Winterfeld, U., Pomar, L., Lambelet, V., Cleary, B., O'Shaughnessy, F., Passier, A., Richardson, J. L., Hompes, T., & Nordeng, H. (2021). Mental health status of pregnant and breastfeeding women during the COVID-19 pandemic-A multinational cross-sectional study. Acta Obstetricia et Gynecologica Scandinavica, 100(7), 1219–1229. https://doi.org/10.1111/aogs.14092
Chen, J., Guo, Y., Liao, Z., Xia, W., & She, S. (2020). Does pregnancy make women more cautious and calm? The impact of pregnancy on risk decision-making. Judgment and Decision Making, 15(5), 807-822. Retrieved from https://econpapers.repec.org/article/jdmjournl/v_3a15_3ay_3a2020_3ai_3a5_3ap_3a807-822.htm
Chhabra, J., McDermott, B., & Li, W. (2020). Risk factors for paternal perinatal depression and anxiety: A systematic review and meta-analysis. Psychology of Men & Masculinities, 21(4), 593–611. https://doi.org/10.1037/men0000259
Cohen, S., Kamarck, T., & Mermelstein, R. (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24(4), 385–396. https://doi.org/10.2307/2136404
da Matta, A., Gonçalves, F. L., & Bizarro, L. (2012). Delay discounting: Concepts and measures. Psychology & Neuroscience, 5(2), 135-146. http://dx.doi.org/10.3922/j.psns.2012.2.03
Davenport, M.H., Meyer, S., Meah, V.L., Strynadka, M.C., & Khurana, R. (2020). Moms are not ok: Covid-19 and maternal mental health. Frontiers in Global Women’s Health, 1(1), 1-6. https://doi.org/10.3389/fgwh.2020.00001
Doyle, M., Carballedo, A., & O'Keane, V. (2015). Perinatal depression and psychosis: An update. BJPsych Advances, 21(1), 5-14. doi:10.1192/apt.bp.112.010900
Effective Health Care Program. (2019, January 11). Maternal and fetal effects of mental health treatments in pregnant and breastfeeding women: A systematic review of pharmacological interventions. https://effectivehealthcare.ahrq.gov/products/mental-health-pregnancy/protocol.
Farrell, R., Dolgin, N., Flocke, S., Winbush, V., Mercer M.B., & Simon, C. (2011). Risk and uncertainty: Shifting decision making for aneuploidy screening to the first trimester of pregnancy. Genet Med, 13, 429–436.https://doi.org/10.1097/GIM.0b013e3182076633
Field, T. (2017). Prenatal Depression Risk Factors, Developmental Effects and Interventions: A Review. Journal of Pregnancy and Child Health, 4(1), 301. https://doi.org/10.4172/2376-127X.1000301
Figueiredo, B., & Conde, A. (2011). Anxiety and depression in women and men from early pregnancy to 3-months postpartum. Archives of Women's Mental Health, 14(3), 247–255. https://doi.org/10.1007/s00737-011-0217-3
Harris, C. R., Jenkins, M., & Glaser, D. (2006). Gender differences in risk assessment: Why do women take fewer risks than men? Judgment and Decision Making, 1(1), 48–63. Retrieved from https://psycnet.apa.org/record/2007-04381-005
Hartley, C. A., & Phelps, E. A. (2012). Anxiety and decision-making. Biological Psychiatry, 72(2), 113–118.https://doi.org/10.1016/j.biopsych.2011.12.027
Hodgkinson, E.L., Smith, D.M. & Wittkowski, A. (2014). Women’s experiences of their pregnancy and postpartum body image: a systematic review and meta-synthesis. BMC Pregnancy Childbirth, 14, 330.https://doi.org/10.1186/1471-2393-14-330
Holmes, T. H., & Rahe, R. H. (1967). The social readjustment rating scale. Journal of Psychosomatic Research, 11(2), 213–218. https://doi.org/10.1016/0022-3999(67)90010-4
Huang, F., Wang, H., Wang, Z., Zhang, J., Du, W., Su, C., Jia, X., Ouyang, Y., Wang, Y., Li, L., Jiang, H., & Zhang, B. (2020). Psychometric properties of the perceived stress scale in a community sample of Chinese. BMC Psychiatry, 20, 130. https://doi.org/10.1186/s12888-020-02520-4
Kaplan, B. A., Amlung, M., Reed, D. D., Jarmolowicz, D. P., McKerchar, T. L., & Lemley, S. M. (2016). Automating scoring of delay discounting for the 21-and 27-item monetary choice questionnaires. The Behavior Analyst, 39(2), 293-304. https://doi.org/10.1007/s40614-016-0070-9
Kazemi, A., Ghaedrahmati, M. & Kheirabadi, G. (2021). Partner’s emotional reaction to pregnancy mediates the relationship between pregnancy planning and prenatal mental health. BMC Pregnancy Childbirth, 21, 168.https://doi.org/10.1186/s12884-021-03644-5
Kirby, K. N., & Maraković, N. N. (1996). Delay-discounting probabilistic rewards: Rates decrease as amounts increase. Psychonomic Bulletin and Review, 3(1), 100−104. doi:10.3758/bf03210748
Kita, S., Haruna, M., Matsuzaki, M., & Kamibeppu, K. (2020). Does Antenatal Social Support Affect the Relationships Between Intimate Partner Violence During Pregnancy and Perinatal Mental Health? Violence Against Women, 26(6–7), 573–589. https://doi.org/10.1177/1077801219835052
Kroenke, K., Spitzer, R. L., & Williams, J. B. W. (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613. https://doi.org/10.1046/j.1525-1497.2001.016009606.x
Kusev, P., Purser, H., Heilman, R., Cooke, A.J., Schaik, P.V., Baranova, V., Martin, R., Ayton, P. (2017). Understanding risky behavior: The influence of cognitive, emotional and hormonal factors on decision-making under risk. Frontiers in Psychology, 8, 102. https://doi.org/10.3389/fpsyg.2017.00102
Laplante, D.P., Brunet, A., Schmitz, N., Ciampi, A., & King, S. (2008). Project Ice Storm: Prenatal Maternal Stress Affects Cognitive and Linguistic Functioning in 5½ -Year-Old Children. Journal of the American Academy of Child & Adolescent Psychiatry, 47(9), 1063-72. doi: 10.1097/CHI.0b013e31817eec80
Lau Y. (2012). Traditional Chinese Pregnancy Restrictions, Health-Related Quality of Life and Perceived Stress among Pregnant Women in Macao, China. Asian Nursing Research, 6(1), 27–34. https://doi.org/10.1016/j.anr.2012.02.005
Lee, S., Ayers, S., & Holden, D. (2016). Decision-making regarding place of birth in high-risk pregnancy: a qualitative study. Journal of Psychosomatic Obstetrics & Gynecology, 37(2), 44-50. https://doi.org/10.3109/0167482X.2016.1151413
Lejuez, C.W., Read, J.P., Kahler, C.W., Richards, J.B., Ramsey, S.E., Stuart, G.L., Strong, D.R., Brown, R.A. (2002). Evaludation of a behavioral measure of risk taking: the balloon analogue risk task (BART). Journal of Experimental Psychology: Applied, 8(2), 75-84. doi: 10.1037//1076-898X.8.2.75
Li, A., Peng, Y. & Xiong, G. (2015). Are Pregnant Women More Foresighted? The Effect of Pregnancy on Intertemporal Choice [in Chinese]. Acta Psychologica Sinica, 47(11), 1360-1370. http://journal.psych.ac.cn/xlxb/CN/10.3724/SP.J.1041.2015.01360
Li, Y., Long, Z., Cao, D., & Cao, F. (2017). Social support and depression across the perinatal period: A longitudinal study. Journal of Clinical Nursing, 26(17-18), 2776–2783. https://doi.org/10.1111/jocn.13817
Lighthall, N.R., Mather, M., & Gorlick, M.A. (2009). Acute stress increases sex differences in risk seeking in the balloon analogue risk task. PLoS ONE, 4(7): e6002. doi:10.1371/journal.pone.0006002
Liu, C., Spector, P. E., & Shi, L. (2007). Cross‐national job stress: a quantitative and qualitative study. Journal of Organizational Behavior, 28(2), 209-239. doi: 10.1002/job.435
Liu, X., Chen, M., Wang, Y., Sun, L., Zhang, J., Shi, Y., Wang, J., Zhang, H., Sun, G., Baker, P.N., Luo, X., & Qi, H. (2020). Prenatal anxiety and obstetric decisions among pregnant women in Wuhan and Chongqing during the COVID-19 outbreak: a cross-sectional study. An International Journal of Obstetrics and Gynaecology, 127(10), 1229-1240. doi: 10.1111/1471-0528.16381.
Lyerly, A. D., Mitchell, L. M., Armstrong, E. M., Harris, L. H., Kukla, R., Kuppermann, M., & Little, M. O. (2007). Risks, values, and decision making surrounding pregnancy. Obstetrics and gynecology, 109(4), 979–984. https://doi.org/10.1097/01.AOG.0000258285.43499.4b
Madsen, S.A. (2019). Men and perinatal depression. Trends Urology & Men Health, 10(2), 7-9. https://doi.org/10.1002/tre.681
Marteau, T. M., & Bekker, H. (1992). The development of a six-item short-form of the state scale of the Spielberger State–Trait Anxiety Inventory (STAI). British Journal of Clinical Psychology, 31(3), 301–306. https://doi.org/10.1111/j.2044-8260.1992.tb00997.x
Mazur, J. E. (1987). An adjusting procedure for studying delayed reinforcement. In M. L. Commons, J. E. Mazur, J. A. Nevin, & H. Rachlin (Eds.), Quantitative analyses of behavior: Vol. 5. The effect of delay and of intervening events on reinforcement value (pp. 55-73). Hillsdale, NJ: Erlbaum.
McDonald, K., Amir, L.H. & Davey, MA. (2011). Maternal bodies and medicines: a commentary on risk and decision-making of pregnant and breastfeeding women and health professionals. BMC Public Health, 11, S5. https://doi.org/10.1186/1471-2458-11-S5-S5
Miguel, P.M., Pereira, L.O., Silveira, P.P., & Meaney, M.J. (2019). Early environmental influences on the development of children's brain structure and function. Developmental Medicine & Child Neurology, 61(10), 1127-33. https://doi.org/10.1111/dmcn.14182
Mischel, W., Ebbesen, E.B., Zeiss, A.R. (1972). Cognitive and attentional mechanisms in delay of gratification. Journal of Personality and Social Psychology, 21(2), 204-218. doi: 10.1037/h0032198
Moran, A. C., Sangli, G., Dineen, R., Rawlins, B., Yaméogo, M., & Baya, B. (2006). Birth-preparedness for maternal health: findings from Koupéla District, Burkina Faso. Journal of health, population, and nutrition, 24(4), 489–497. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3001153/
Napso, T., Yong, H.J., Lopez-Tello, J., & Sferruzzi-Perri, A.N. (2018). The Role of Placental Hormones in Mediating Maternal Adaptations to Support Pregnancy and Lactation. Frontiers in Physiology, 9, 1091. https://doi.org/10.3389/fphys.2018.01091
Niemeyer, H., Bieda, A., Michalak, J., Schneider, S., & Margraf, J. (2019). Education and mental health: Do psychosocial resources matter? SSM-Population Health, 7(100392), 100715. https://doi.org/10.1016/j.ssmph.2019.100392
O'Connor, E., Rossom, R. C., Henninger, M., Groom, H. C., & Burda, B. U. (2016). Primary Care Screening for and Treatment of Depression in Pregnant and Postpartum Women: Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA, 315(4), 388–406. https://doi.org/10.1001/jama.2015.18948
Oshri, A., Hallowell, E., Liu S., MacKillop, J., Galvan, A., Kogan, S.M., & Sweet, L.H. Socioeconomic hardship and delayed reward discounting: Associations with working memory and emotional reactivity. Developmental Cognitive Neuroscience, 37, 100642. https://doi.org/10.1016/j.dcn.2019.100642
Pailing, A.N., & Reniers, R.L.E.P. (2018). Depressive and socially anxious symptoms, psychosocial maturity, and risk perception: Associations with risk-taking behaviour. PLoS ONE 13(8), e0202423. https://doi.org/10.1371/journal.pone.0202423
Pike, A.C., Anet, A., Peleg, N., & Robinson, O.J. (2021). Catastrophizing is associated with reduced risk-taking. https://doi.org/10.17605/OSF.IO/Z2RGK
Reimers, S., Maylor, E.A., Stewart, N., & Chater, N. (2009). Associations between a one-shot delay discounting measure and age, income, education and real-world impulsive behavior. Personality and Individual Differences, 47(8), 973-978. https://doi.org/10.1016/j.paid.2009.07.026
RStudio Team (2020). RStudio: Integrated Development for R. RStudio, PBC, Boston, MA. http://www.rstudio.com/.
Russell, H., & Banks, J. (May, 2011). Pregnancy and employment: A literature review. HSE Crisis Pregnancy Programme and the Equality Authority. Retrieved from https://www.esri.ie/system/files?file=media/file-uploads/2015-07/BKMNEXT189.pdf
Sevin, E. & Ladwein, R. (2008). To start being….The anticipation of a social role through consumption in life transition: the case of the first-time pregnancy. NA - Advances in Consumer Research, 35, 325-332. Retrieved from https://www.acrwebsite.org/volumes/13565/volumes/v35/NA-35
Sheeba, B., Nath, A., Metgud, C.S., Krishna, M., Venkatesh, S., Vindhya, J., & Murthy, G.V.S. (2019). Prenatal Depression and Its Associated Risk Factors Among Pregnant Women in Bangalore: A Hospital Based Prevalence Study. Frontiers in Public Health, 7, 108. https://doi.org/10.3389/fpubh.2019.00108
Sidebottom, A. C., Harrison, P. A., Godecker, A., & Kim, H. (2012). Validation of the Patient Health Questionnaire (PHQ)-9 for prenatal depression screening. Archives of women's mental health, 15(5), 367–374. https://doi.org/10.1007/s00737-012-0295-x
Solivan, A.E., Xiong, X., Harville, E.W., & Buekens, P. (2015). Measurement of perceived stress among pregnant women: a comparison of two different instruments. Maternal and Child Health Journal, 19(9), 1910–1915. https://doi.org/10.1007/s10995-015-1710-5
Spielberger, C. D., Gorsuch, R. L., Lushene, R., Vagg, P. R., & Jacobs, G. A. (1983). Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press.
Starcke, K., & Brand, M. (2012). Decision making under stress: a selective review. Neuroscience and Biobehavioral Reviews, 36(4), 1228–1248. https://doi.org/10.1016/j.neubiorev.2012.02.003
Steele, L. S., Dewa, C. S., Lin, E., & Lee, K. L. (2007). Education level, income level and mental health services use in Canada: associations and policy implications. Healthcare policy/ Politiques de Santé, 3(1), 96–106. Retrieved from https://pubmed.ncbi.nlm.nih.gov/19305758/
Walder, D.J., Laplante, D.P., Sousa-Pires, A., Veru, F., Brunet, A., & King, S. (2014) Prenatal maternal stress predicts autism traits in 6½ year-old children: Project Ice Storm. Psychiatry Research, 219(2), 353-60. https://doi.org/10.1016/j.psychres.2014.04.034
Wallsten, T. S., Pleskac, T. J., & Lejuez, C. W. (2005). Modeling Behavior in a Clinically Diagnostic Sequential Risk-Taking Task. Psychological Review, 112(4), 862–880. https://doi.org/10.1037/0033-295X.112.4.862
Wang, W., Bian, Q., Zhao, Y., Li, X., Wang, W., Du, J., Zhang, G., Zhou, Q., & Zhao, M. (2014). Reliability and validity of the Chinese version of the Patient Health Questionnaire (PHQ-9) in the general population. General Hospital Psychiatry, 36(5), 539–544. https://doi.org/10.1016/j.genhosppsych.2014.05.021
Wu, F., Lin, W., Liu, P., Zhang, M., Huang, S., Chen, C., Li, Q., Huang, W., Zhong, C., Wang, C., Wang, Y., & Chen, Q. (2021). Prevalence and contributory factors of anxiety and depression among pregnant women in the post-pandemic era of COVID-19 in Shenzhen, China. Journal of Affective Disorders, 291(1), 243-251. https://doi.org/10.1016/j.jad.2021.05.014
Yan, H., Ding, Y., & Guo, W. (2020). Mental health of pregnant and postpartum women during the coronavirus disease 2019 pandemic: A systematic review and meta-analysis. Frontiers in Psychology, 11, 3324-36. https://doi.org/10.3389/fpsyg.2020.617001
Yang, T., & Huang, H. (2003). An epidemiological study on stress among urban residents in social transition period [in Chinese]. Chinese Journal of Epidemiology, 24(9), 760-764. Retrieved from http://chinaepi.icdc.cn/zhlxbx/ch/reader/view_abstract.aspx?file_no=20030906&flag=1
Yirmiya, K., Yakirevich-Amir, N., Preis, H., Lotan, A., Atzil, S., & Reuveni, I. (2021). Women's depressive symptoms during the Covid-19 pandemic: The role of pregnancy. International journal of environmental research and public health, 18(8), 4298. https://doi.org/10.3390/ijerph18084298
Zheng, X., Shu, L., Zhang, A., Huang, G., Zhao, J., Sun, M., Fu, Y., Li, H., & Xu, D. (1993). Application report of the State-Trait Anxiety Inventory (STAI) used in Changchun, China [in Chinese]. Chinese Mental Health Journal, 7(2), 60-62. doi: CNKI:SUN:ZXWS.0.1993-02-003
Zhou, R., Myung, J.I., Pitt, M.A. (2021). The scaled target learning model: revisiting learning in the balloon analogue risk task. Cognitive Psychology, 128, 1-16. https://doi.org/10.1016/j.cogpsych.2021.101407
Zhou, Y., Shi, H., Liu, Z., Peng, S., Wang, R., Qi, L., Li, Z., Yang, J., Ren, Y., Song, X., Zeng, L., Qian, W., & Zhang, X. (2020). The prevalence of psychiatric symptoms of pregnant and non-pregnant women during the COVID-19 epidemic. Translational Psychiatry, 10, 319. https://doi.org/10.1038/s41398-020-01006-x
Zhou, Y., Wang, R., Liu, L., Ding, T., Huo, L., Qi, L., Xiong, J., Yan, J., Zeng, L., Yang, J., Song, S., & Dai, G. (2021). The impact of lockdown policy on depressive symptoms among pregnant women in China: mediating effects of internet use and family support. Global Health Research and Policy, 6, 11. https://doi.org/10.1186/s41256-021-00193-4
